Seniorly Resource Center
Learn how to navigate senior living, from what to look for in a community, how to finance, move in tips and more.
Senior Living Guides
See all Senior Living GuidesCity Guides
See all City GuidesCaregivers
See all Caregivers
Explore Topics

City Guides
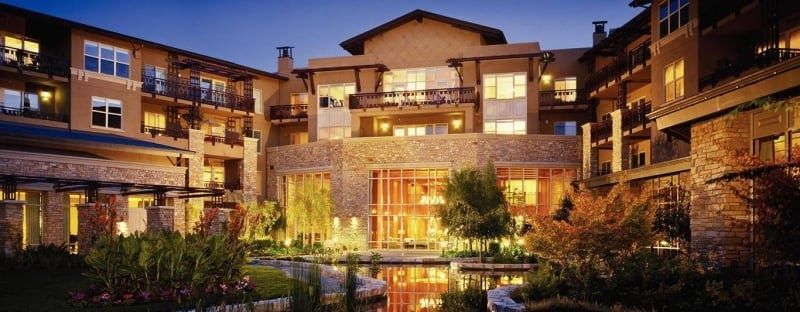
See what different cities have to offer seniors, from senior living options to art, music, and culture.

Senior Living Guides
Learn about different senior living options, common terms, and more so that you can make the best decisions for yourself or your loved ones.

Health and Lifestyle
Explore senior health topics, fun activities in your area, travel tips and more to make the most of senior life.

Caregivers
Find resources and support for caregivers so that you can offer your loved one your best self every day.
Voices
Hear from senior living experts, families, and seniors themselves about senior care and how to find the best fit.

Seniorly News
Get the latest on Seniorly and stay on top of our efforts to make finding senior living simpler.
Sign up for our Healthy Aging Handbook
Seniorly’s Senior Living experts created a comprehensive handbook to help people age happily while ensuring they love where they live. Enter your email address below to receive your copy and learn more about Healthy Aging and Senior Living.*
*By submitting your email address above, you consent to receive occasional email communications from Seniorly, including educational content and tips, newsletters, and other relevant updates and offerings. You can unsubscribe at any time and we will never sell or distribute your email address to a third party. You can view our Privacy Policy here.